Shoulder bursitis or subacromial bursitis is a common condition affecting the shoulder that falls under the umbrella term Subacromial Shoulder Pain.
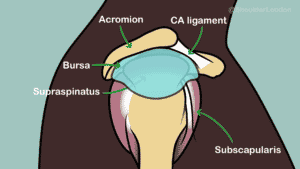
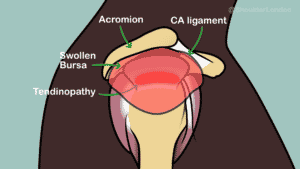
Bursas are normal structures, and we have them all over our body where tendons glide under other structures such as skin or bone. The subacromial bursa is a normal structure that sits on top of the rotator cuff tendons, under the acromion, and helps the rotator cuff tendons to glide under the acromion bone. Bursitis describes the inflammation of a bursa.
Is subacromial bursitis the same as impingement?
Shoulder impingement is a term used to describe a mechanical phenomenon where the rotator cuff tendon at the top of the shoulder and the subacromial bursa get pinched as the arm is lifted due to a bony spur under the acromion and thickening of the coracoacromial ligament. Subacromial bursitis can occur with or without shoulder impingement.
What causes shoulder bursitis to flare up?
There are various things that can cause shoulder bursitis to flare up. Bursitis is usually seen in the 40 to 65yr age group but can be seen in younger patients who have jobs that require lots of overhead activity such as plumbers or electricians. Sudden change in activity with increased repetition of overhead movement such as taking on DIY or deciding to paint a room all in one go are examples of some mechanical causes of subacromial bursitis.
Some patients have immune or rheumatological disorders that can cause bursitis to flare up.
Inflammatory shoulder conditions such as calcific tendonitis in the rotator cuff tendons can cause the bursa to become inflamed.
In some patients there is no obvious cause or trigger to their bursitis.
What are the symptoms of subacromial bursitis?
Patients with subacromial bursitis often complain of pain over the deltoid region of the shoulder. The pain usually occurs as they lift their arm over shoulder height so reaching for things in a high cupboard or shelf can often be uncomfortable.
It is not uncommon for patients with shoulder bursitis to have pain if they sleep on the affected side.
How is shoulder bursitis diagnosed?
Getting an accurate shoulder diagnosis requires taking a careful history of the patient’s problem, symptoms, and medical history. The patient then needs to be examined, and investigations ordered depending on the proposed problem. The bursa is a soft tissue so it cannot be seen on xray or CT scan. Diagnosing shoulder bursitis requires either ultrasound or MRI. We often prefer to use an MRI scan for the shoulder as it doesn’t require moving the painful shoulder, it is less operator dependent, and both the surgeon and the radiologist can review the images to double check the diagnosis.
How can I self-manage my bursitis?
You can prevent bursitis by avoiding suddenly taking on repetitive overhead tasks. DIY for instance should be balanced by taking regular breaks to rest the shoulder. If you already have a flare up of shoulder bursitis, ice can help to settle the inflammation. You can find a useful shoulder ice pack here. If icing doesn’t help, then simple over the counter anti-inflammatories such as ibuprofen and painkillers such as paracetamol can help but you may need to seek medical advice if you haven’t used these before. You can find out more about managing shoulder pain here.
The British Elbow & Shoulder Society has provided a great patient resource for those with subacromial shoulder pain which includes and information leaflet and a home exercise programme that could help your bursitis.
How is shoulder bursitis treated?
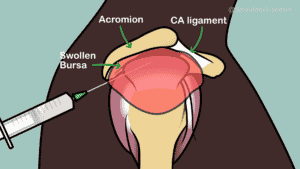
If self-management doesn’t control your pain from shoulder bursitis, then you need to seek medical attention to get an accurate diagnosis and consider medical treatment. The first line of treatment for subacromial bursitis is a subacromial space steroid injection to help settle the inflammation in the shoulder. This should then be followed a week later with a course of physiotherapy to strengthen the rotator cuff muscles as they often are week after a bout of shoulder pain. Physiotherapy for rotator cuff strengthening should be exercise based and should last at least 12 weeks to see any benefit.
What is shoulder bursitis surgery?
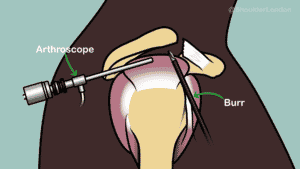
If non-operative management as above doesn’t work, then surgery is often a last resort. The operation for subacromial bursitis is called a subacromial decompression. This operation is done as a day-case, key-hole operation, and I recommend that this be done with the patient awake under regional anaesthesia.
Patients go home on the day of the operation with a temporary sling. Once the nerve block has worn off (usually around 24hrs later) the sling can be removed, and the arm can be used. Physiotherapy should start soon after surgery and usually lasts for 12 weeks. The recovery from this operation is relatively quick and there is a high success rate when there is careful patient selection. This operation is only usually needed a handful of times a year as most patients get better without surgery.